What Happens to the Body After Gallbladder Removal?
3 Conditions That May Follow – Why Surgery Should Be Carefully Considered
Gallbladder removal, medically known as cholecystectomy, is one of the most common surgeries worldwide. It is often recommended for gallstones, inflammation, or infection that causes pain and digestive problems. While many people recover well and live normal lives afterward, removing the gallbladder does change how the digestive system works. Understanding these changes—and the possible conditions that may follow—can help patients make informed decisions and manage their health after surgery.
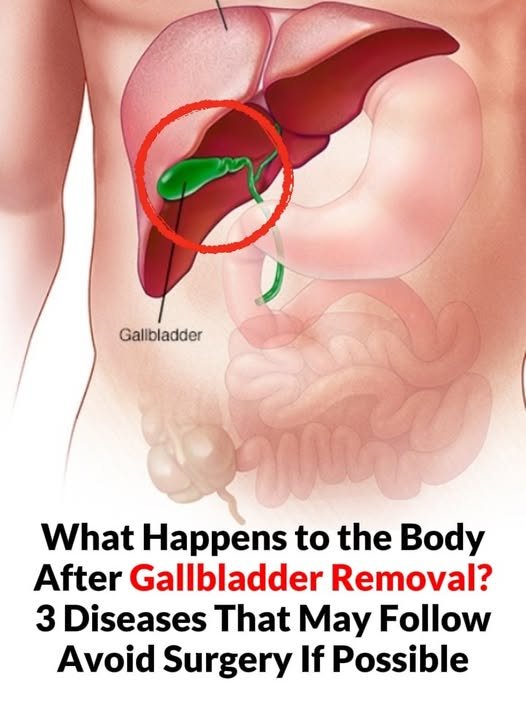
The Role of the Gallbladder in Digestion
The gallbladder is a small organ located beneath the liver. Its main function is to store and concentrate bile, a digestive fluid produced by the liver. Bile helps break down fats so they can be absorbed by the body.
When the gallbladder is removed, bile no longer gets stored. Instead, it flows continuously from the liver directly into the small intestine. While the body can adapt to this change, the digestive process becomes less efficient, especially when digesting fatty foods.
What Changes After Gallbladder Removal?
After surgery, many people notice changes such as:
- Difficulty digesting fatty or greasy meals
- Bloating or gas
- Diarrhea or loose stools
- Abdominal discomfort after eating
For some, these symptoms are temporary. For others, they may persist and lead to longer-term conditions.
1. Post-Cholecystectomy Syndrome (PCS)
One of the most common issues after gallbladder removal is Post-Cholecystectomy Syndrome. This term describes a group of digestive symptoms that continue or appear after surgery.
Symptoms may include:
- Chronic abdominal pain
- Indigestion
- Nausea
- Diarrhea
- Acid reflux
PCS can occur due to bile flowing too freely into the intestines or stomach, irritating the digestive lining. In some cases, symptoms may be linked to underlying digestive conditions that were not diagnosed before surgery.
2. Bile Acid Diarrhea
Without the gallbladder regulating bile release, excess bile can enter the intestines too quickly. This may lead to bile acid diarrhea, a condition characterized by frequent, watery stools.
This happens because bile acids irritate the colon, increasing water secretion and speeding up bowel movements. Over time, this can interfere with nutrient absorption and affect daily quality of life.
Dietary adjustments, such as reducing fatty foods and eating smaller meals, may help manage symptoms. In more persistent cases, doctors may recommend medications that bind bile acids.
3. Increased Risk of Digestive Disorders
Some studies suggest that gallbladder removal may be associated with a higher risk of certain digestive issues over time, including:
- Acid reflux (GERD)
- Irritable bowel syndrome (IBS)
- Small intestinal bacterial overgrowth (SIBO)
Continuous bile flow can disrupt the balance of gut bacteria and irritate the digestive tract. While not everyone develops these conditions, the risk highlights the importance of long-term digestive care after surgery.
Should Gallbladder Surgery Be Avoided?
Gallbladder removal can be life-saving and necessary, especially in cases of severe infection, blockage, or repeated gallstone attacks. However, it should not always be viewed as the first or only option.
In mild or early cases, doctors may explore alternatives such as:
- Dietary changes
- Weight management
- Medications to dissolve certain gallstones
- Monitoring without immediate surgery
The key is individual evaluation. What works for one person may not be safe or effective for another.
Life After Gallbladder Removal
Many people live healthy, active lives without a gallbladder. The body can adapt, especially with supportive habits such as:
- Eating balanced, lower-fat meals
- Avoiding large, heavy portions
- Staying hydrated
- Following medical advice for digestive symptoms
Final Thoughts
Gallbladder removal is common and often effective, but it is not without consequences. Understanding how the body changes—and the possible conditions that may follow—allows patients to make informed decisions and prepare for life after surgery.
If surgery is recommended, discussing risks, benefits, and alternatives with a qualified healthcare professional is essential. When possible, preserving natural organ function is beneficial, but when surgery is necessary, proper post-operative care can make a significant difference in long-term health.